A 35 YEAR OLD FEMALE WITH FEVER AND THROMBOCYTOPENIA
This is an online e log book to discuss our patients' deidentified health data shared after taking his/ her/ guardians consent. Here we discuss our individual patients' problems through a series of inputs from an available global online community of experts with an aim to solve those patients' clinical problems with the collective current best evidence based inputs. This e- log also reflects a patient centered learning portfolio.
NAME : G PRAVALLIKA
ROLL NO: 41
3RD SEMESTER
A 35 years old woman presented to the casuality with chief complaints of fever, cold , vomiting and cough.
HISTORY OF PRESENT ILLNESS :
A 35 year old woman presented to the casuality with chief complaints of fever since 1 week, cough since 1 week and vomiting since that morning on 17/10/21.
She has been having low grade , intermittent fever with no diurnal variation and non productive cough. She also had 3 episodes of non projectile, non bilious vomiting with no hematemesis.
HISTORY OF PAST ILLNESS:
NO H/O Diabetes, hypertension, tuberculosis, asthma, epilepsy, thyroid, CAD, CVD.
The patient contracted some bacterial infection at 5 years of age. Her left upper and lower limb were paralysed due to the infection to the extent that normal function of the above limbs was affected.
She was taken to a hospital in Tirupati for a surgery to resolve her left upper limb function but the surgery was unsuccessful.
She was on oral medication for 2 years after which she regained some power in her Left UL and LL and was able to perform regular functions.
PERSONAL HISTORY :
Mixed diet
Unmarried
Normal appetite
Adequate sleep
Regular bladder and bowels movements
No addictions
Occupation: Stopped schooling in 1st grade , only does household chores.
FAMILY HISTORY :
No history of diabetes, hypertension, asthma, TB, CAD, CVD, polio.
GENERAL EXAMINATION :
Patient was conscious, coherent, co - operative.
Well oriented to time, place, and person.
Moderately built and moderately nourished.
No pallor
No clubbing
No cyanosis
No lymphadenopathy
No edema
VITALS :
PR : 95 bpm, regular
Bp : 100/80 mm of Hg
Respiratory rate: 20/ min
GRBS : 138mg /dl
Temperature: 98.6 degrees F
SpO2: 99%
SYSTEMIC EXAMINATION:
PER ABDOMINAL EXAMINATION :
INSPECTION -
Shape - Scaphoid
Umbilicus - inward
Movements with respiration - equal in all quadrants rises with inspiration and falls during expiration .
No visible pulsations
No visible scars or sinuses seen
No engorged veins
PALPATION :
No local rise of temperature
No tenderness in any quadrants of abdomen, liver and spleen - impalpable ( no organomegaly)
PERCUSSION :
- No dullness of abdomen
AUSCULTATION :
Bowel sounds present
CVS EXAMINATION :
S1, S2 heard
No murmurs
RESPIRATORY SYSTEM EXAMINATION :
Trachea - midline
Bilateral air entry present
Normal Vesicular breath sounds heard
No additional sounds
CNS EXAMINATION :
Gait - (circumduction) abnormal due to left foot abnormality
Sensations - present
Cranial nerves - intact
Reflexes - brisk
Neck stiffness: No
Kerning’s sign: No
Finger nose coordination: Yes
Kneel Heel coordination: Yes
OBSTETRIC HISTORY :
G0, unmarried.
INVESTIGATIONS ORDERED :
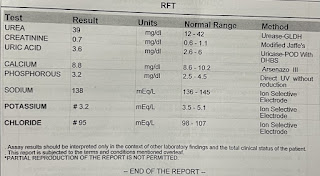
ECG, CXR - PA, USG Abdomen, Hemogram, LFT, RFT, Complete urine examination, Dengue serology.
HEMOGRAM on 18/10
PROVISIONAL DIAGNOSIS: Dengue NS1 positive.
TREATMENT:
1. Plenty of fluids
2. IVF 20 NS - @125ml/hour
10 RL - @ continuous infusion
3. Inj. PANTOP 40 mg IV/ OD
4. Inj. ZOFER 4mg IV/TID
5. Syrup. AMBROXOL 10 ml PO/ TID w/ 1 glass of water
6. Tab. DOLO 650 mg PO/SOS
7. W/F Bleeding manifestations
8. Platelets , PCV 12th hourly
9. Monitor vitals
10. I/O Charting
Blood transfusion was done when the platelet count was 40,000 lakh / cu mm.
The patient is doing well now and she's being discharged today (25/10)











Comments
Post a Comment